Previously, we have talked about our friends at the Department of Radiology at Stanford University in Palo Alto, California and their amazing use of the Depth 3-Dimensional (D3D) Augmented Reality system for CT Scan reviews of breast cancer. Well, we follow very closely the people who work with Augmented Reality, and we have exciting updates! This time, we’re talking about the potential of Augmented Reality and mammography.

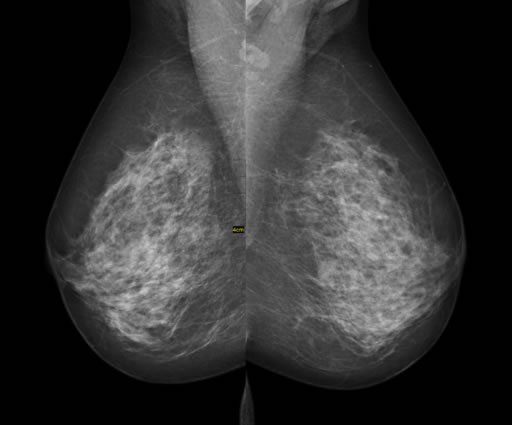
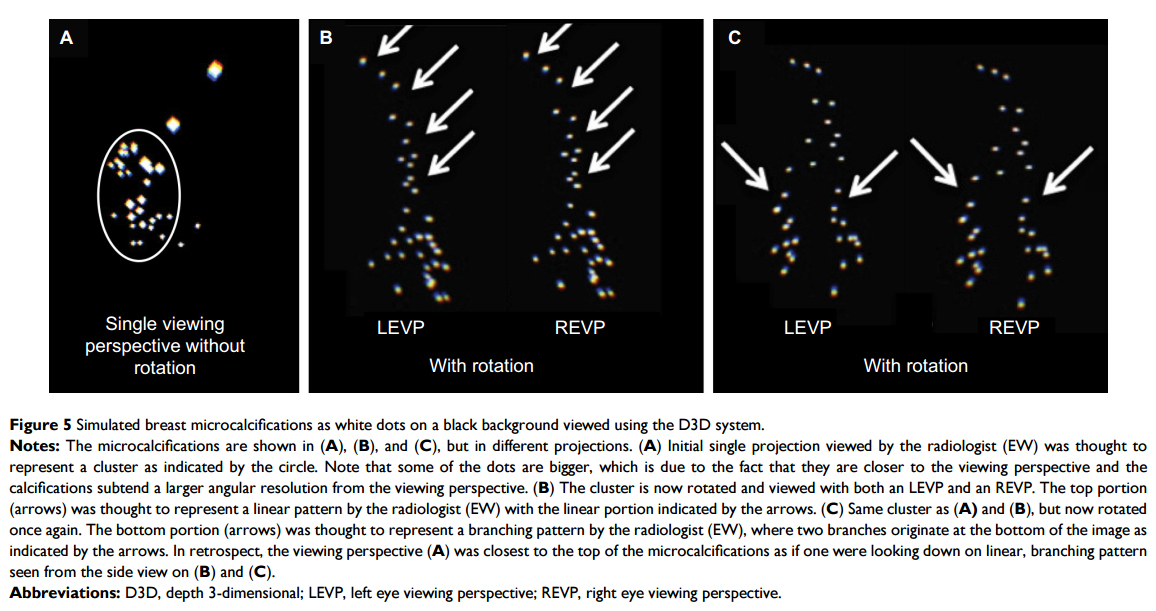
It’s no secret that regular, annual mammography studies are recommended for women. However, while 2000 women that undergo screening with mammography will prolong their life 10 years, 10 of those 2000 will undergo unnecessary treatments for benign findings, and another 10 will receive false positive results. With that said, it’s clear that mammography has room for improvement. Mammography is great because it can detect suspicious microcalcifications that could be associated with breast cancer in asymptomatic patients. For example, a linear and branching distribution of microcalcifications is suspicious for ductal carcinoma in situ, but standard mammography may not reveal the true linear and branching pattern because of the limitations of a 2D viewpoint.
It’s not easy to analyze a 3D pattern on a 2D image, right?
Taking this in account, a full 3D viewing of the aforementioned calcifications has the advantage of reducing mistakes during the diagnosis process. In this study, images from a simulated dataset of microcalcifications were viewed using D3D software to evaluate the presence of a branched or linear pattern in an Augmented Reality setting. This AR setting was achieved through the use of a wearable AR headset, with the point of view controlled by a joystick allowing the physician to “fly through” the 3D model. An expert imagenologist visualized the microcalcifications in 2D, initially classifying them as a cluster, an indeterminate diagnosis for cancer. However, after reviewing the microcalcifications with D3D, microcalcifications were revealed to have a linear pattern, and after further rotation, were classified as having a branching pattern, which is highly suspicious for ductal carcinoma in situ (DCIS) breast cancer.
3D Mammography is already being performed around the world. However, the usage of AR is special because it provides an immersive and flexible point of view. We would love to see some more in-depth studies about this, but for now, we really appreciate any initiative to improve conventional mammography. What are your thoughts? Tell us in the comments section!
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4984822/pdf/mder-9-277.pdf









[…] Education is surely a place where this technology could be useful, but the possibilities don’t end there. Clinical practice could use it, too. One problem that patients and doctors face today is false negative results from main core biopsies. There are no definitive numbers for all main core biopsies, but in one study of breast cancer, over 2% of all the 998 biopsies presented false negatives, and for others, it can be much higher–up to 8.9% when certain methods of core biopsy are used. These numbers might not sound too high, but false negative results often delay treatment for patients, allowing metastasis of the cancer, especially in more aggressive forms. The Zstack technology could be the key to earlier diagnosis of cancers, if it’s applied to clinical histology, by allowing the physician to navigate through the 100% of the biopsy sample, establish new protocols and signs to determine malignancy, like they already do for mammography assessment. […]