Laparoscopic surgery has proven to be a blessing for patients and surgeons alike. It’s a minimally invasive surgery, which allows procedures to be done in less time and recuperations are faster than ever before. A surgery as complicated as gallbladder surgery (laparoscopic cholecystectomy), which is done when there’s a need to remove this oftentimes undervalued organ, has its own risks, some of them are inherent to any kind of surgery such as infection, bleeding, or risks from the general anesthetic. According to the National Health Service in the United Kingdom, other risks like bile leakage or injury to the bile duct occur in 1 out of 100 and 1 out of 500 cases, respectively, and are a bit more complicated, putting the patient’s life at risk and jeopardizing their quality of life.

Obviously, risks cannot be avoided for every patient as every aspect is different and there are inherent risks. But does this mean that it cannot be avoided or at least can we try a different approach to avoid it? That’s the question that researchers from the University Hospital of Strasbourg at France asked themselves, and they came up with a very interesting system that uses Near-infrared cholangiography (NIR-C), which is a technology that allows radiation-free biliary anatomy exploration in real time, X-ray Intraoperative Cholangiography (IOC), Magnetic Resonance Cholangiopancreatography (MRC) with Virtual Reality (VR) for preoperatory exploration, and then Augmented Reality (AR) for intraoperative navigation.
How was this done? Fifty-eight patients scheduled for cholecystectomy for a gallbladder lithiasis were selected. The patients underwent VR surgical planning from 3D models built from MRC imaging. After the preoperative planning, patients were then prepped for laparoscopic cholecystectomy and at the moment of anesthesia induction, indocyanine green was administered intravenously. The 3D model used for preoperative planning is also used for AR intraoperative navigation, which is complemented by overlaying it onto real-time images obtained by NIR-C images through the laparoscope camera before and after the Calot triangle dissection (hence the indocyanine green). At the end of the procedure, IOC is performed to assess the success of the procedure.

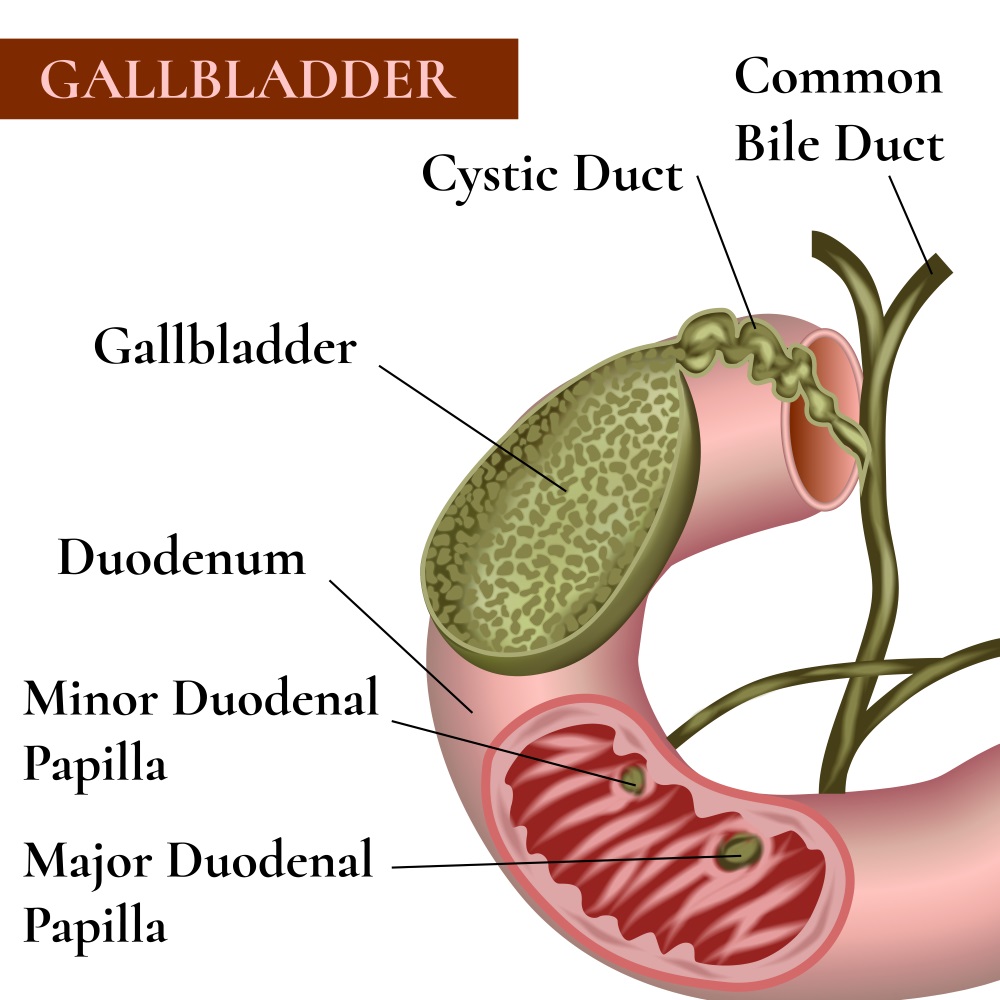
The combination of all the imagenologic techniques offered the following results: 3D VR planning allowed the identification of 12 anatomical variants in 8 patients (only 7 were correctly reported by radiologists). One of the most important anatomical references, the cystic-common bile duct junction, was visualized in 100% of cases with VR, 98.15% with NIR-C, and 96.15% with IOC. What does this mean? The merge of this multimodal imaging of biliary anatomy in the form of a protocol enhances the possibilities of this procedure towards a higher precision cholecystectomy.

Evidently, not everything was perfect since a tendency to perform a Laparoscopic retrograde Cholecystectomy (fundus first approach) was detected, and as you may know, this is controversial. But anyway, there are many more studies that need to be done to prove the impressions that this feasible study showed, but at this very moment the perception is that these visualization techniques could be used to reduce the likelihood of biliary injuries, improving the technique and making it a safer procedure for the patients. More aspects need to be taken in account, such as its feasibility in more austere environments. We cannot wait to learn more about the development of this protocol!
Let us know your thoughts in the comments section!








