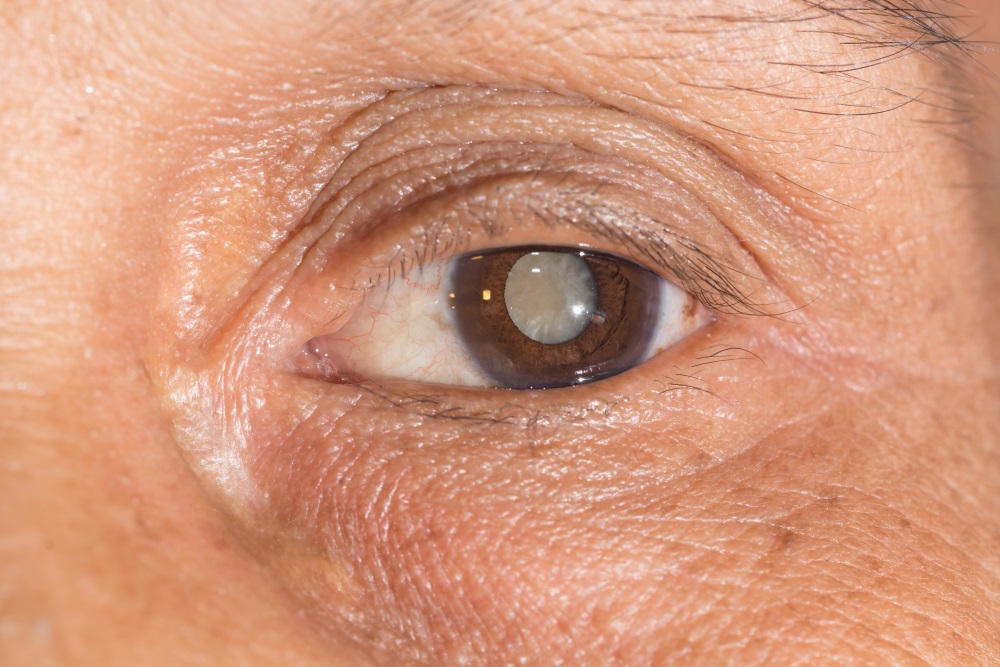
We’ve talked before about augmented reality for medical training: it seems like a great alternative to traditional training because it allows theoretical training to be hands-on, without using real patients until the trainee is comfortable. It polishes their skills in a setting that resembles the actual procedure more than any other simulation on the market. While there has been resistance against AR’s use in other procedures–with patients, for example–most people are in agreement that it’s good for medical training. Its benefits are evident, particularly in the field of eye surgery. For example, phacoemulsification is the latest procedure to treat cataracts. The surgery consists of emulsifying the eye’s internal lens using ultrasound, and retrieving the emulsification later. The fluids in the anterior chamber are then replaced with a balanced solution, and a lens implant is placed.
It goes without saying that this is a delicate procedure. The eye is a sensitive, fragile area! However, it’s one of the most frequently used procedures in ophthalmology, and training for it is therefore imperative. With this in mind, researchers from the Universiti Malaysia Perlis and the Department of Ophthalmology from Hospital Tuanku Fauziah, both located in Perlis, Malaysia, have designed a new and exciting augmented/mixed reality training for the procedure, called the Phacoemulsification Cataract Surgery Training Simulator. (Reminder: If you would like to review the differences between Virtual and Augmented Reality you can do it HERE.)

The simulator consists of a screen which displays a realistic 3D model of the surgical field for the phacoemulsification, a stylus with haptic feedback, and a keyboard and mouse to adjust the view. In order to test the simulator, they divided 16 participants, 10 being full-fledged, experienced ophthalmologists and the other 6 being residents, into two groups. Both groups performed the same virtual phacoemulsification procedure, subdivided into four main surgical steps: corneal incision, capsulorhexis, phacoemulsification, and intraocular lens implantation. The score was evaluated objectively based on several parameters, including precision of each incision, force applied, time taken, number of touches applied, and percentage of cataract fragments retrieved–all parameters that could not accurately be assessed in a real surgery.

Results showed up that the group consisting of experienced ophthalmologists performed better than the residents for exception of one parameter: percentage of removed cataract fragments. This results correlates with the usual performance expected in the real procedure, correlating
this device to the actual operation, making it ideal for the training of this new ophthalmologists, it could also serve as an assessment tool for them, giving them parameters to be evaluated and for their tutors to find out when they are truly ready to perform the procedure in an objective way while forming better doctors along the way.

Certainly, this isn’t the first of the training devices that augmented reality has made possible. Seeing so many new devices has allowed us to understand better how the world of AR is shaping the landscape of medicine–and we’re excited about it! We can’t wait to see what the next few years will offer us! Let us know what you think in the comments section!








