There are 50,000 new amputations in the US each year according to the National Center for Health Statistics, and about 1:4 are upper extremity amputees. Around 10,000 people lose their hands every year in US and 77% of these amputations are because of trauma. Certainly, each of these patients suffer a significant quality of life setback when they lose a hand. Even if the patients receive a fully-fledged late generation prosthetic hand, we must not forget about phantom limb pain, post-traumatic stress disorder, not to mention just having to cope with the limitations on their usual daily activities and chores.
And obviously, the deprivation of the sense of touch is a significant life-change. Think about not being able to caress the face of your son, feel the warmth of a cup of coffee or the sensation of silk in your hands; all of this is lost for these patients, for life. Because of this, researchers at the Institute of Neurorehabilitation Systems, Clinics for Trauma, Orthopedic and Plastic Surgery and the University Medical Center Göttingen of Georg-August University at Göttingen, Germany have developed GLIMPSE, a Google Glass application that connects to a prosthesis via Bluetooth transmitting information for EMG signals, aperture, force and contact through Augmented Reality (visual alerts) and sound (bone conduction transducer).
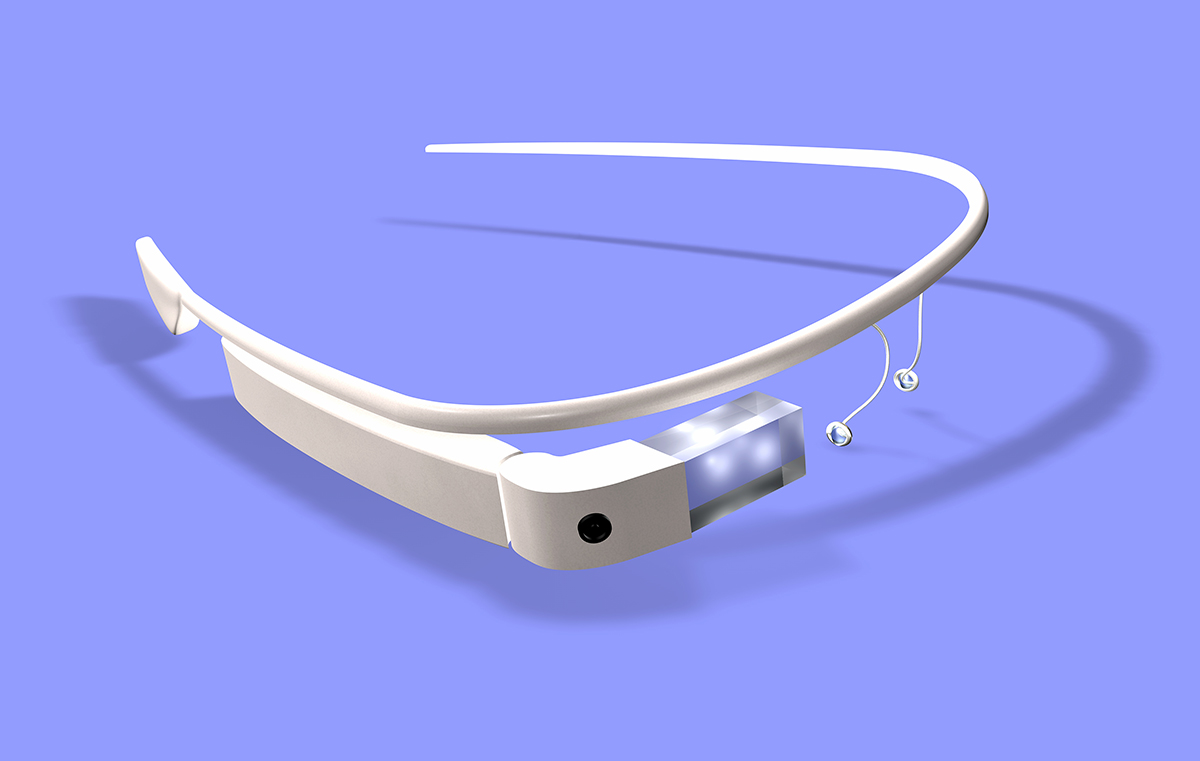
The GLIMPSE application was tested with a group of healthy subjects with prostheses. One group received the GLIMPSE feedback and another group did not. A modified clothespin test was used with different levels of difficulty. The number of unsuccessful trials, time to accomplish the task, and the subjective ratings of the relevance of the feedback were some of the outcomes that were evaluated. Results showed that there was virtually no difference in performance while doing a simple task, but the gap increased significantly on the performance of more complex tasks, like using pins of different resistances. The group that received the GLIMPSE feedback for the more complex tasks had consistently better results while performing the action.

It was determined that the GLIMPSE’s supplemental feedback could be useful in more demanding tasks. Interestingly, all patients integrated the supplemental GLIMPSE feedback with their own intrinsic sources, like vision and muscle proprioception allowing them to develop their own idiosyncratic strategies to accomplish the task. This means that GLIMPSE’s feedback is intuitive, easy to adapt and ready to exploit from the first minute of use. The successful GLIMPSE test is definitely a nice first step in gaining new and advanced sensory feedback for prostheses through the use of AR.
Obviously, GLIMPSE is a relatively simple development in the vast array of technologies for sensory feedback; however, the integration of newer technologies such as AR into applications such as GLIMPSE is something medical innovators need to be thinking about – and now! And don’t forget, Augmented Reality is a fairly economic solution that offers a different perspective and heightened benefits to many of the therapies that have been done in this arena in the past.
What do you think? Do you believe that AR can change the landscape of prostheses technology? Let us know in the comments section!!
Source: https://www.ncbi.nlm.nih.gov/pubmed/28355147