Skin cancer, as with any cancer, is a health issue not only in the United States – but the entire world. Obviously some cancers are more aggressive than others, but many wouldn’t disagree that Melanoma is one of the most vicious of them. Some of the statistics on Melanoma are baffling! For example, it is brought to our attention by the Skin Cancer Foundation that one person dies of melanoma every 54 minutes! It is also said that 87,110 new cases of invasive melanoma will be diagnosed in the U.S. alone in 2017. These are worrying numbers, but of course there, are measures that can be taken, such as regular daily use of sunscreen (SPF 15 or higher). Proper use of sunscreen reduces the risk for squamous cell carcinoma by about 40 percent, and the risk of melanoma dwindled by 50 percent.

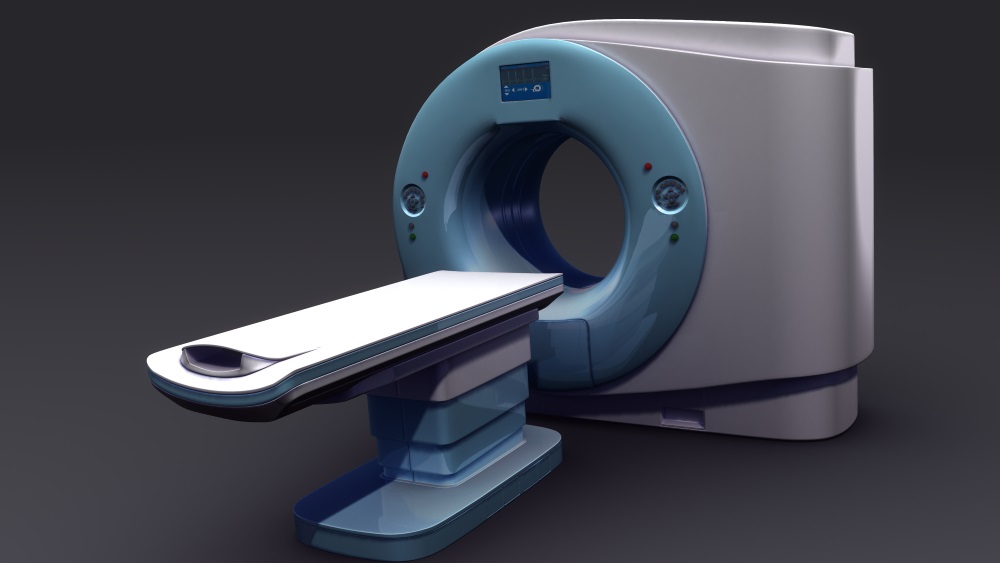
Is it enough? No, it isn’t. The estimated 5-year survival rate is about 98%, but if detected early, this rate decreases to 62% with lymph node compromise, and 18% when it is metastasized. Every single effort is being made to improve the risk of developing this kind of cancer and to improve its survival rate. Because of this reason, researchers from the Melanoma Center in Amsterdam, the Netherlands, and the Melanoma Institute at Sydney, Australia have developed a feasible study that implements the use of Mixed Reality technology with Single Photon Emission Computed Tomography and regular Computed Tomography (SPECT/CT) imaging for sentinel node (SN) biopsy for melanoma or Merkel cell carcinoma.
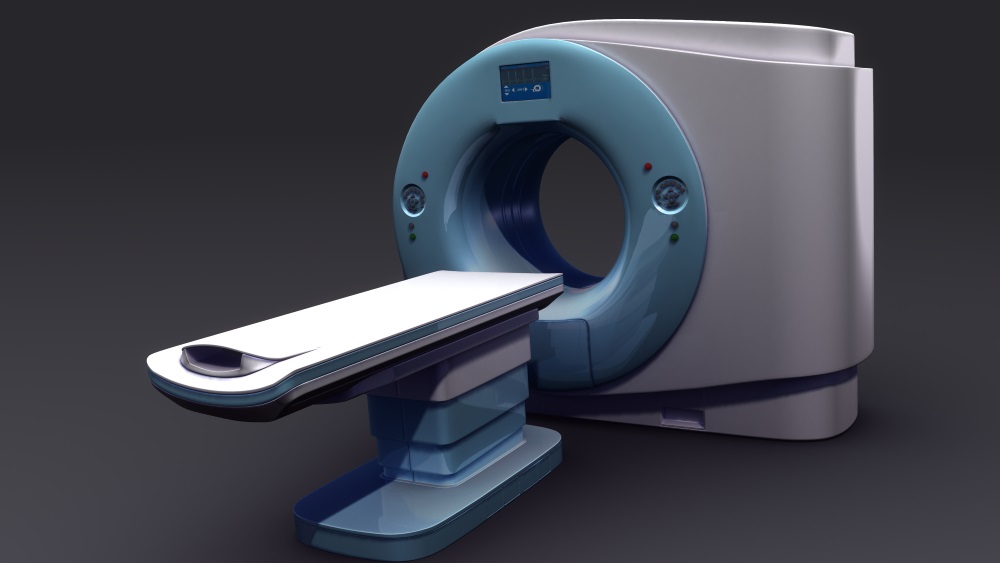
How does this work? This study took four melanoma patients and one Merkel cell carcinoma patient, all of which were cases scheduled for lower extremity wide re-excision of the primary lesion site and SN biopsy. SPECT/CT images were acquired with a reference target fixed on the iliac spine (for MR display reasons). During the surgery, a sterilized reference target was fixed on the same place, allowing for MR navigation by using a tablet with an integrated camera, which portrayed the previously acquired images over the operatory field in real time.

In four out of the five patients, navigation towards the preoperatively defined SN was succesful by using the MR system. Importantly, the average navigational error sagittally was 8.0 mm, and 8.5 mm coronally. Even though this is important, it didn’t make the study impossible and it’s also worth noting that by polishing the system it is totally corregible, making this feasible study a success in its own terms.

In conclusion, the Intraoperative navigation for melanoma or Merkel cell carcinoma surgery is possible by using the merge of SPECT/CT imaging and MR. By doing this, an interactive 3D roadmap towards the SN or SNs in the groin is provided to the surgeon intraoperatively in real time. By implementing this procedure, we will be making an impact (by how much is yet to be determined) on the speed, effectiveness, and recuperation times for the patients that undergo this technique. However, as we always say here at ARinMED, further studies and technical optimization of the technique is required before this technology can become a gold standard.
Please let us know your thoughts in the comments section!