A Paravertebral Sympathetic Plexus Block (PSPB) is a procedure in which dye and pain medication is administered into the spine between lumbar vertebrae at the prevertebral and paravertebral sympathetic ganglia. The procedure can be either diagnostic or for treatment purposes, depending on the needs of the patient. It can be used to diagnose and/or treat pain stemming from a wide variety of conditions, including phantom limb pain, herpes zoster, acute pancreatitis, pancreatic cancer, pain from upper-abdominal viscera cancers, and even inoperable peripheral vascular vasospastic diseases of the lower limbs. Of course, this is not an easy procedure–any time a needle is in the spine, it’s risky–and it’s not indicated for every patient. However, it is a good option for patients who have not responded to other methods of pain relief. Because of the high risk of complications like nontarget needle localization, which can cause pain and discomfort to the patient for long periods of time, image-guidance is recommended to reduce mistakes, but there is currently no consensus about which image guidance system should be used.
Fluoroscopy, computed tomography (CT), and magnetic resonance imaging (MRI) are some of the imaging methods that doctors frequently use for this procedure, and there are pros and cons to each. MRI, at least on paper, is best because it has the highest contrast for soft tissues, true multiplanar capabilities, and it doesn’t use radiation, which lowers the exposure of both patient and physician to harmful radiation. Therefore, researchers at the Russel H. Morgan Department of Radiology and Radiological Science and physicians from the Johns Hopkins University School of Medicine developed a feasibility study to test the initial technical performance of an Augmented Reality MRI technique as a new approach for perineural injections of the thoracic, lumbar, and hypogastric sympathetic ganglia.

The team performed this study using twelve non embalmed human cadavers to perform a total of 23 bilateral PSPB procedures at the thoracic, lumbar, and hypogastric levels. The cadavers underwent an imaging process through a 1.5 T MRI scanner (Magnetom Espree, Siemens Healthcare) before an interventional radiologist used a MRI-compatible needle to perform each of the procedures. The radiologist was using an Augmented Reality-assisted MRI navigation system. This system works by using high-resolution 3D turbo spin-echo MRI data sets, obtained from thoracic, lumbar, and sacral vertebrae, to gain visualization of the paravertebral sympathetic plexus, allowing the radiologist perfect localization of the puncture target. This visualization allows the radiologist to navigate the needle quickly and precisely through the spine. These 3D images were then sent to the navigation module for interactive 3D evaluation of the anatomy using the system’s DICOM viewer function.

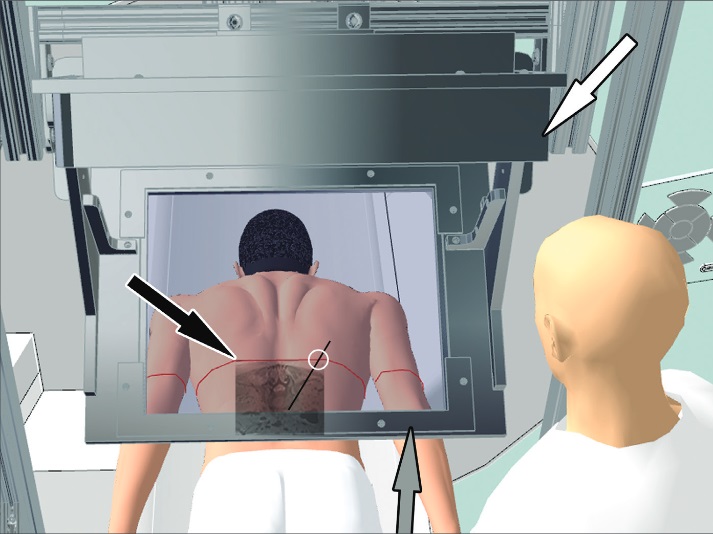
Using this navigation software, the radiologist marked the target point for the final needle tip location as well as the desired entry point through the skin. After both points were identified, the system plotted the needle’s path and, after the image was obtained and the specimen was moved below the image-overlay navigation system, the radiologist was able to align the needle perfectly with the position of the navigation system, and the MRI image containing the target and its virtual needle path were projected through a semitransparent mirror. By observing the cadaver through the semitransparent mirror of the image-overlay system, the AR navigation technology is the first of its kind (Fig. 2). The image-overlay navigation system was positioned to optimize the location, size, and skin contour between the MRI image and the cadaver specimen, resulting in a flawless completion of the procedure.
All 46 planned punctures were carried out successfully in all the cadavers and at all spinal levels, each with correct injectant delivery and perineural spread for all targets. MRI used to provide confirmation of the correct positioning of the needle. Unfortunately, an average of two intermittent MRI control steps were required to place a needle, and with nine trajectory adjustments of the needle during the process. However, there were no misses reported. Of course, more studies need to be done in order to confirm that this method is safe. Remember, there’s not even a defined criteria that MRI is the gold standard for PSPB, and with its many risks (non-successful injectant delivery, pleural puncture, renal puncture, and others), this method still cannot guarantee safety. In vivo studies are also needed to determine how factors such as patient respiration might affect the actual procedure, but as we previously said, this is a feasible method because it allows a strong visualization of the anatomy, reducing the chances of failure, and allows correct visualization of the injectants, permitting the physician to confirm procedure success.
We at ARinMED are so happy to hear that augmented reality is influencing such a delicate procedure. We hope to see this advancement help alleviate the extreme pain of patients with conditions for which PSPB is indicated. By reducing the risks and increasing the accuracy, this procedure becomes safer and more efficient, and its future looks bright! Do you agree? Let us know in the comments section below!







